Breast Cancer: Surgery
Surgery is a common treatment for breast cancer. It’s done to remove as much of the cancer as possible. You have many surgical options. The type of surgery you need depends on:
-
The size of the breast lump or tumor and where it is in your breast
-
The type of breast cancer
-
If the cancer has spread within your breast or has spread beyond your breast to lymph nodes or other parts of your body
-
The size of your breasts
-
Your preference
-
Other health problems you have such as diabetes or heart disease
-
Your overall health
-
Family history and your genes
The two main surgeries to remove breast cancer are:
In addition to breast surgery, your surgeon will look for spread into nearby lymph nodes.
Breast reconstruction is surgery to rebuild the breast shape. It can be started during the surgery to remove the cancer or at a later time. If you think you want breast reconstruction, talk with your healthcare provider about it before having surgery. Some people choose not to have reconstruction.
Breast-conserving surgery
This type of surgery is also called breast-sparing surgery, lumpectomy, quadrantectomy, partial mastectomy, or segmental mastectomy. The surgeon takes out only the cancer lump and an edge (margin) of healthy tissue around it. Most of the breast remains intact.
Most women get radiation therapy after breast-conserving surgery. This is done to destroy cancer cells that may not have been removed during surgery. In some cases, chemotherapy, hormone therapy, or both are given after breast-conserving surgery.
Whether breast-conserving surgery is a good option for you depends on many factors. Studies have shown that people who have the same stage of breast cancer and have breast-conserving surgery with radiation have the same survival rates as those who have mastectomy. Many people prefer this type of surgery instead of having their whole breast removed. You and your surgeon will discuss what option is best for you. Not all people are able to have breast-conserving surgery.
There are two main types of breast-conserving surgery: lumpectomy and partial (segmental) mastectomy.
A lumpectomy removes the breast cancer and part of the normal tissue around it. Some of the lymph nodes under the arm might be removed to see if the cancer has spread (sentinel lymph node biopsy, see below), or all of the lymph nodes may be removed (axillary dissection).
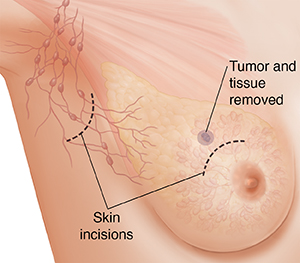 |
| Lumpectomy. |
A partial (segmental) mastectomy removes the breast cancer and a larger part of the normal breast tissue around the cancer. The surgeon may also remove some of the lymph nodes under the arm. (See section on sentinel lymph node biopsy below.)
Mastectomy
Mastectomy is surgery to remove the breast. A mastectomy may be needed for someone who has:
-
Cancer in more than one part of the breast and it cannot all be removed with a single incision (cut)
-
A history of radiation therapy to the affected breast or chest area
-
A small breast with a large tumor in it
-
Inflammatory breast cancer
-
A connective tissue disease, which means radiation may cause major problems
-
A current pregnancy, because the radiation needed after breast-conserving surgery could harm the unborn baby
-
Some tumor left over from previous breast-conserving surgery
-
Genetic mutation (BRCA). This may increase your risk for a second breast cancer.
Some people may choose mastectomy instead of breast-conserving surgery for personal reasons. Some people choose to have a double mastectomy (removal of both breasts) if they are at high risk for getting breast cancer a second time.
There are four main types of mastectomy. Each has its own benefits and risks.
A total (or simple) mastectomy removes the entire breast. This includes the nipple, areola, the covering of the main chest muscle, and most of the skin. The surgeon may also remove some of the lymph nodes under the arm to see if the cancer has spread. (See section on sentinel lymph node biopsy below.)
A skin-sparing mastectomy removes the same amount of breast tissue and the nipple and areola, but it leaves most of the skin. This may be an option if the tumor is small or not close to the surface. Breast reconstruction is done as part of this surgery.
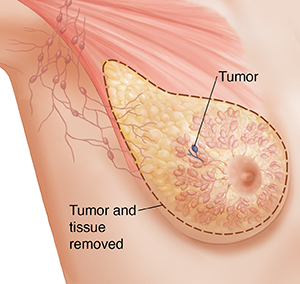 |
| Simple mastectomy. |
A modified radical mastectomy removes the entire breast. This includes the skin, nipple, covering of the main chest muscle, and areola. Lymph nodes under the arm are also removed. (See section on axillary lymph node dissection below.)
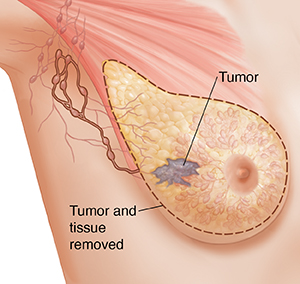 |
| Modified radical mastectomy. |
A radical mastectomy is also called a Halsted radical mastectomy. It removes the entire breast, including the nipple, areola, and skin. All the lymph nodes under the arm (axillary lymph nodes) and the chest wall muscles under the breast are also removed.
A radical mastectomy is very rarely needed. Still, it might be done to treat a large tumor that's growing into the chest muscles.
Sentinel lymph node biopsy
The lymphatic system is part of the immune system. It's one of the pathways cancer cells can use to travel to other parts of the body (metastasize). It’s made up of lymph nodes and vessels that carry lymph fluid throughout the body. Lymph nodes are small round organs along the vessels that filter the lymph fluid as it flows through.
The lymph nodes under the arm are called the axillary lymph nodes. They drain lymph from the arms, most of the breast, the neck, and the underarm areas. Breast cancer may spread to these lymph nodes. It can then enter the lymphatic system and spread to other parts of the body.
The sentinel lymph node is the node the cancer reaches first. A special procedure can be done to find this node or nodes so they can be taken out and checked for cancer cells. (There can be more than one sentinel lymph node.) It can be done at the same time as a lumpectomy or a mastectomy. It might be done when the cancer is small and there's no sign that it has spread to the lymph nodes.
To do a sentinel lymph node biopsy, a specially trained surgeon injects a radioactive substance, blue dye, or both near the tumor. The dye travels through the lymph to the sentinel node. This node can then be found and removed. It’s sent to a lab to see if it has cancer cells in it.
If the sentinel node doesn’t have cancer, then it's unlikely that there's cancer in the other axillary nodes. No more nodes need to be removed. Having your underarm lymph nodes removed can lead to serious side effects. (See section on axillary lymph node dissection below.)
Axillary lymph node dissection
This surgery takes out (dissects) all the lymph nodes under the arm (the axillary lymph nodes). It can be done at the same time as breast-conserving surgery or mastectomy, or later as a second surgery. It might be needed if:
-
Cancer is found in three or more sentinel lymph nodes (described above)
-
A lymph node biopsy showed cancer
-
Chemotherapy was given before surgery, but the sentinel lymph node biopsy still shows cancer cells
-
Advanced stage breast cancer where sentinel lymph node biopsy won't impact prognosis or treatment
This surgery can have some serious long-term side effects. Tests are done beforehand to make sure it's needed.
Risks of breast cancer surgery
All surgery has some risks. The risks of breast cancer surgery include:
Breast-conserving surgery may cause:
-
Short-term swelling, bruising, and pain in the breast
-
Change in breast size and shape
-
Clear fluid trapped in the wound (seroma) that may need to be drained
A serious risk of having many lymph nodes removed is swelling of the arm, hand, chest, and neck (lymphedema). This can cause:
-
A tight feeling in the arm or decreased sensation along the arm
-
Pain
-
Redness
-
Decreased flexibility of the arm, hand, and wrist
There may be other risks depending on your overall health and the type of surgery done. Talk with your healthcare team about the risks of your specific surgery.
Questions to ask your healthcare provider before surgery
Your healthcare team will talk with you about the surgery options that are best for you. You may want to bring a family member or close friend with you to appointments. Write down questions you want to ask about your surgery. You might want to ask:
-
Exactly what type of surgery will be done?
-
What will be done during surgery?
-
How long will the surgery take?
-
How long will I need to stay in the hospital?
-
What are the risks and possible side effects of the surgery? Are there long-term side effects?
-
Will the surgery leave scars? What will they look like?
-
How will my breast or chest look and feel after surgery?
You may also want to ask your healthcare provider other questions, such as:
-
Which type of surgery do you advise for me? Why?
-
Where will the cut (incision) be? How much breast tissue will be removed?
-
Will any lymph nodes be removed?
-
Will I be able to have breast reconstruction if I have a mastectomy?
-
Do you advise breast reconstruction to be done at the same time of the mastectomy? Or should it be done at a later date?
-
Will I need more treatment after surgery, like radiation, hormone therapy, or chemotherapy?
-
What type of follow-up care will I need?
-
How long does it usually take to recover?
-
When can I go back to my normal activities?
-
Will my insurance cover surgery? How much will I need to pay?
Getting ready for your surgery
Before surgery, tell your healthcare team if you are taking any medicines. This includes over-the-counter medicines, vitamins, herbs, and other supplements. It also includes illegal drugs and marijuana. This is to make sure you’re not taking anything that could affect the surgery. After you've discussed all the details with the surgeon, you'll sign a consent form that says that the healthcare provider can do the surgery.
You’ll also meet the anesthesiologist. This is the healthcare provider in charge of the medicine that helps you sleep and feel no pain during surgery. You can ask questions about the anesthesia and how it will affect you.
After your surgery
You may have to stay in the hospital for a few days, depending on the type of surgery you had. You may want to talk with your insurance company before your surgery.
Your healthcare providers will explain the side effects you can expect with each type of surgery. They can also suggest ways to help prevent or manage these side effects. It is important that you let your healthcare provider know about any changes or problems you notice.
After breast surgery, it's common to have:
-
Pain. For the first few days after surgery, the incision will hurt. Your pain can be controlled with medicine. Talk with your healthcare provider or nurse about your options for pain relief. Some people don’t want to take pain medicine, but doing so can help your healing. If you don’t control pain well, you may not want to cough or move, which you need to do as you recover from surgery.
-
Tightness and swelling in your skin. The skin near your breast may feel tight. Sometimes your arm and shoulder muscles will feel stiff, too. This will get better as you heal. You'll be given exercises to help regain full motion in your shoulder. Don't start the exercises until your healthcare provider says it's OK.
-
Fatigue. It's normal to feel very tired or weak for a while. The amount of time it takes to recover from surgery is different for each person, but this usually gets better with time.
Recovering at home
When you get home, you may get back to light activity. But you should not do any strenuous activity for 6 weeks. Your healthcare team will tell you what kinds of activities are safe for you while you recover.
After breast cancer surgery, you will have a bandage (dressing) over the place where you had surgery. It's important to keep the surgical area clean and dry. You'll be told how to bathe and when you can shower. If adhesive strips are used, they should be kept dry. They will fall off in a few days.
You may also have tubes in your chest. These are called drains. They remove blood and fluids that build up during the normal healing process. You may have to empty and measure the fluid. The drains stay in for about 2 weeks, or until only a small amount of fluid is draining.
Your healthcare provider or nurse will give you written instructions on how to care for your incision, change your bandage, and manage the drains. You’ll also be told when to call your healthcare provider or nurse about a problem. Be sure you understand the instructions. Also be sure you know how to get in touch with your healthcare provider.
You may be told to start exercises the day after your surgery, or at a later time. These exercises may include doing things like flexing your fingers and touching your hand to your shoulder. Ask if there are any exercises or activities you should not do.
Losing one or both of your breasts can be emotionally difficult. After surgery, you and your partner should take the time to talk about how you feel. You may feel that you need counseling. Ask your healthcare provider for the names and locations of support groups or counselors if you feel you need one.
Possible complications after surgery
After surgery, you may have any of the below. Talk with your healthcare team about what you should watch for and what you need to tell them about.
-
Stiffness in your underarm after lymph node removal. Gentle exercises and massage therapy can help with stiffness. Don’t use hair removal creams, strong deodorants, or shave under your arm for about 2 weeks after surgery.
-
Lack of feeling in the skin on your breast, chest, or upper arm. When your breast is removed, nerves must be cut. This may cause short-term numbness. Often, most of the feeling slowly returns. It can take a year or two after surgery. Some numbness may be permanent.
-
Phantom breast sensations. You may feel like your breast is still there. People who lose limbs often have this feeling, too. It often gets better or goes away over time.
-
Shift in weight or feeling off-balance. If you had large breasts, losing one or both of them can make you feel off-balance. It can also make your neck or back hurt. This tends to get better as you adjust to the changes in your body.
-
Constipation. You may have constipation from using a certain type of pain medicine (narcotics), from not moving much, or from not eating much. Talk with your healthcare provider or nurse about getting more dietary fiber or using a stool softener.
-
Lymphedema. If you’ve had your underarm lymph nodes removed or treated with radiation, you may have swelling in your chest, arm, and hand on the side where you had surgery. While this is normal right after surgery, it can later become a long-term problem. Be sure you understand what to watch for and what to do to help keep this from happening.
Follow-up care
Your healthcare provider will tell you when to return for a follow-up visit. During this visit, your incision will be checked. If needed, the stitches will be removed.
You may need radiation treatment or some other kind of treatment after surgery. Your healthcare provider will talk with you about this and when it will start.
When to call your healthcare provider
Talk with your healthcare provider about problems you should watch for. Call right away if you have any of these problems after surgery:
-
Any unusual bleeding or bleeding that soaks through the bandage
-
Signs of infection around the incision, such as redness, drainage, warmth, and pain
-
Fever of 100.4°F (38°C) or higher, or as advised by your healthcare provider
-
Chills
-
Cough or shortness of breath
-
Trouble passing urine or changes in how your urine looks or smells
-
Swelling in your hand, arm, or chest that gets worse or is not getting better a week or two after surgery
-
Pain, redness, swelling, or warmth in an arm or leg
-
Any other concerns
Know what problems to watch for and when you need to call your healthcare provider. Also be sure you know what number to call to get help after office hours and on weekends and holidays.