Gastroesophageal Reflux in Children
What is gastroesophageal reflux in children?
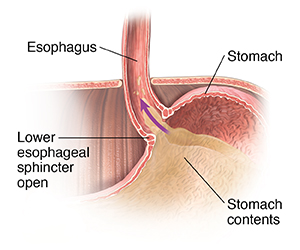
Gastroesophageal refers to the stomach and esophagus. The esophagus is the tube that connects the throat to the stomach. Reflux means to flow back or return. Reflux happens because the lower esophageal sphincter in babies opens easily. This allows the acidic stomach juices, food, and fluids to flow back into your child’s esophagus.
Reflux can happen at any age, but it’s common in babies. It is often a short-term (temporary) problem. But if it becomes a long-term problem, it is called gastroesophageal reflux disease (GERD).
What causes reflux in a child?
Reflux is often caused by problems with the lower esophageal sphincter. This is a muscle at the bottom of the esophagus. Normally, it opens to let food into the stomach and closes to keep food in the stomach. When this muscle relaxes too often or for too long, acid goes back into the esophagus. This causes nausea, vomiting, and heartburn.
As babies digest their food, the lower esophageal sphincter may open. This lets stomach contents go back up into your child’s esophagus. Sometimes the contents go all the way up. This causes your baby to vomit. Sometimes acid or material can pass into the windpipe (trachea) and cause coughing or infection. Other times, the contents may only go part of the way up the esophagus. This can cause heartburn or breathing problems. Or it may not cause symptoms.
What are the symptoms of reflux in a child?
Symptoms can occur a bit differently in each child. They can include:
-
Belching
-
Choking
-
Coughing often
-
Fussiness around mealtimes
-
Gagging
-
Getting ear infections often
-
Hiccups
-
Having coughing fits at night
-
Not wanting to eat
-
Rattling sound in the chest
-
Stomachache
-
Wheezing
The symptoms of this condition may be similar to symptoms of other health problems. Have your child see their healthcare provider for a diagnosis.
How is reflux diagnosed in a child?
Your child’s healthcare provider will examine your child and check their health history. Your child may need the following tests to diagnose reflux.
Chest X-ray
A chest X-ray is done to look for signs of aspiration. Aspiration happens when the stomach contents spill into the lungs. This causes breathing problems and lung infections.
Upper GI (gastrointestinal) series
An upper GI series looks at the organs in the upper part of your child’s digestive system. These include the esophagus, stomach, and the first section of the small intestine (duodenum). For this test, your child will swallow barium. This is a chalky white substance that coats the inside of their organs and can be seen on X-rays. Then your child’s healthcare provider will take an X-ray of these organs.
Endoscopy
In this test, a small, flexible tube (endoscope) is used to look at the inside of your child’s digestive tract. This tube has a light and a camera lens at the end of it. During the test, your child may have tissue samples removed from their digestive tract. The samples are sent to a lab to be looked at.
pH testing
This test measures the level of acidity in your child’s esophagus. Sometimes an impedance test is done with the pH test. Impedance measures the flow of acid, nonacid, and air in your child's esophagus.
Gastric emptying studies
This test will show if your child’s stomach contents empty into their small intestine the correct way. Delayed gastric emptying can cause reflux.
Esophageal motility testing
This test, which is also called esophageal manometry, is done to see if your child's esophagus moves (contracts) correctly. During the test, your child's throat is numbed and a probe is placed down the esophagus to judge whether or not it is contracting normally.
How is reflux treated in a child?
Treatment will depend on your child’s symptoms, age, and general health. It will also depend on how severe the condition is.
Most babies with reflux have no symptoms other than spitting up often. As long as these children grow well and don’t have other issues caused by reflux, they don’t need treatment.
Feeding changes
Sometimes reflux can be managed with feeding changes. These changes should be made under the care of your baby’s healthcare provider. These can include:
-
Hold your baby upright for 30 minutes after feedings. Ask your child’s healthcare provider about the best position for your baby to sleep.
-
Keep the nipple of the bottle filled with milk if you’re bottle-feeding. This can keep your baby from swallowing air when eating. Use a nipple that allows your baby’s mouth to make a good seal with the nipple.
-
Add rice cereal to a feeding. This may help some older babies.
-
Burp your baby several times when bottle-feeding or breastfeeding. Your baby may spit up more often when burping with a full stomach.
-
Make sure your baby’s diaper isn’t too tight. This can make reflux worse.
-
Consider smaller and more frequent feedings.
Medicines
Your baby may need reflux medicine. These medicines can decrease the amount of acid the stomach makes. This will ease the heartburn caused by reflux.
Calorie supplements
Some babies with reflux may vomit often. This can keep them from gaining weight. In this case, your baby’s healthcare provider may suggest the following:
-
Adding rice cereal to your baby’s formula
-
Prescribing a supplement to add calories to your baby’s diet
-
Changing your baby to a milk-free or soy-free formula. Your child’s healthcare provider may do this if they think your child has an allergy.
Tube feedings
Some babies with reflux have other conditions that make them tired. These can include heart disease or being born premature. These babies may not be able to eat much before getting sleepy. Other babies can’t keep a normal amount of formula or breastmilk in their stomachs without vomiting. These babies may do better if they eat a small amount of food continuously.
In these cases, your child’s healthcare provider may advise tube feedings. A tube is placed in your child’s nose and guided through the esophagus and stomach. This is called a nasogastric tube. These tubes can also be used to bypass the stomach if needed. Tube feedings can be done with or in place of bottle-feeding or breastfeeding.
Surgery
In severe cases, your child may need surgery. This surgery is done to reinforce the lower esophageal sphincter. This helps keep the reflux from happening.
What are possible complications of reflux in a child?
Some babies with reflux may not vomit. Instead, their stomach contents may move up and spill over into the windpipe (trachea). This can cause wheezing and pneumonia. In rare cases, this can be life-threatening.
Babies with reflux who vomit often may not gain weight and grow normally. This can cause inflammation (esophagitis) or sores (ulcers) in the esophagus. These ulcers can be painful. They may also bleed. This can lead to anemia. This means too few red blood cells in the bloodstream. Over time, this may cause long-term problems. These can include esophageal narrowing (stricture) and abnormal cells in the lining of the esophagus (Barrett esophagus).
How can I help my child live with reflux?
Many babies with reflux will outgrow it by the time they are age 1. This is when the lower esophageal sphincter becomes stronger. For other babies, feeding and lifestyle changes and medicine can help. Work with your child’s healthcare team to create a care plan for your child.
When should I call my child's healthcare provider?
Call your child’s healthcare provider if your child vomits after every feeding or has new reflux symptoms.
Key points about gastroesophageal reflux in children
-
Gastroesophageal reflux is a digestive disorder.
-
It causes acidic stomach juices, food, and fluids to flow back into your child’s esophagus.
-
This condition can occur at any age, but it’s common in babies.
-
Most babies with reflux have no symptoms other than spitting up often. As long as your baby is growing well and has no other reflux symptoms, they won’t need treatment.
-
Holding your baby upright for 30 minutes after feedings, reducing how much air they swallow, and burping them well during feedings may relieve reflux.
Next steps
Tips to help you get the most from a visit to your child’s healthcare provider:
-
Know the reason for the visit and what you want to happen.
-
Before your visit, write down questions you want answered.
-
At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you for your child.
-
Know why a new medicine or treatment is prescribed and how it will help your child. Also know what the side effects are.
-
Ask if your child’s condition can be treated in other ways.
-
Know why a test or procedure is recommended and what the results could mean.
-
Know what to expect if your child does not take the medicine or have the test or procedure.
-
If your child has a follow-up appointment, write down the date, time, and purpose for that visit.
-
Know how you can contact your child’s healthcare provider after office hours. This is important if your child becomes ill and you have questions or need advice.